User:Stipmraytsat/sandbox
Bile duct cytology is a pathological diagnostic procedure used to examine cell samples obtained from the bile duct to identify structural and genetic abnormalities[1][2]. They provide insights into diagnoses of hepatobiliary diseases, for example, bile duct obstruction, cholangitis or cholangiocarcinoma[3][4].
To obtain cells from the bile duct epithelium, one must visualise the area using endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP)[5][6][7]. Biliary cells are obtained by numerous methods, for example, bile duct aspiration, bile duct biopsy and obtaining bile duct lavage[8][9][10]. Complementary cytogenetic techniques such as fluorescence in situ hybridisation (FISH), next generation sequencing (NGS), and examining microDNA are employed to support primary findings[5][11].
Following a thorough examination of the specimen by pathologists, in conjunction with cytology reports detailing specific biomarkers, doctors can confirm whether the tissue sample is benign or malignant.
However, there results could be misidentified or misclassified, giving rise to wrong results and false diagnoses[12][13].
The emergence of bile duct cytology and visualisation techniques can be traced back to the 1950s, with the introduction of Intravenous cholangiography, percutaneous transhepatic cholangiography (PTC) and secretin test[14][15][16]. In 1975, the first ever documented attempt of ERCP and brush cytology was made[17].
Modern Endoscopic Evaluation of the Bile Duct
[edit]Visualising the bile duct is essential for collecting cells from the bile duct for examination. Endoscopic retrograde cholangiopancreatography (ERCP), endoscopic ultrasound (EUS) and magnetic resonance cholangiopancreatography (MRCP) are widely adopted tools in examining biliary structures. Though they serve the same purpose, different biliary diseases and individuals call for different imaging techniques, often case-sensitive[18]

Endoscopic Retrograde Cholangiopancreatography (ERCP)
[edit]ERCP is an established practice for bile duct endoscopy[5]. It combines endoscopy and fluoroscopy to observe and treat problems within the liver, pancreas and gallbladder. The individual is first put into deep sedation with general anesthesia such as propofol[19][20]. Then, a contrast agent is injected into the individual, and radiographic guidance reveals any abnormal strictures in the biliary tree. A duodenoscope further aids the discovery of minute anomalies within the duct.

Endoscopic Ultrasound (EUS)
[edit]EUS comprises endoscopic visualisation and ultrasound imaging, in observing the bile duct and the surrounding vascular network and lymphatics[6]. Evaluation and curing of pancreaticobiliary disease often necessitate EUS. Commonly used echoendoscopes are radial EUS and linear EUS. Similar to computed tomography (CT), radial EUS provides a 360-degree view in the plane perpendicular to the direction the scope[6]. Alternatively, linear EUS displays an oblique image running parallel to the scope. If the stenosis within the bile duct does not permit passage of standard EUS scopes, mini-probes are used. EUS is considered a salvage therapy when ERCP has failed or when the bile duct had been surgically altered or completely blocked[21].

Magnetic Resonance Cholangiopancreatography (MRCP)
[edit]Contrary to the invasive nature of ERCP and EUS, MRCP does not require injecting contrast agents or using ionising radiation. Overall, it is accurate in evaluating the shapes and sizes of bile duct stones (round or prismatic) and aberrant tissue obstruction within the bile duct[7][22]. Recent advancement in MRCP is tridimensional imaging, which enhances image resolution and allows for a three-dimensional, spatial depiction of the relevant bile duct structures[7].
Cytological Techniques in Bile Duct Analysis
[edit]Sample Collection
[edit]Sample collection is an essential step for examining cells in the bile duct. The most commonly employed methods currently include bile aspiration, bile duct lavage, and brush biopsy[5][8][9].
Bile Aspiration
[edit]Bile aspiration is the most established and convenient method of obtaining cells from the biliary tree for cytodiagnosis. With the aid of a guidewire, the catheter scrapes tissue across the stricture to collect samples. A central suction line is connected to the catheter to aspirate and retrieve samples[8]. Fine needle aspiration is a newer method with improved accuracy. The steel needle has a diameter of 0.8mm and can be advanced up to 10 cm beyond its sheath[23]. By moving back and forth, it collects tissue from the lesion. Afterwards, the needle is withdrawn and proceeds with subsequent staining.
Bile Duct Lavage
[edit]Bile duct lavage is a standard procedure following brush cytology. A catheter injects sterile solution into the bile duct to wash out any fluid and debris[9]. Saline is administered at regular intervals, with 10-15 ml of normal saline injected into the gallbladder. This is followed by a series of saline flushes in 2-3 ml aliquots to irrigate the gallbladder and biliary ducts[24]. It is beneficial as it provides more cells for effectively diagnosing the cytology of indeterminate biliary strictures[25].
Brush Biopsy
[edit]
Brush biopsy is a common sampling technique in cytological examinations[10]. It uses a specially designed brush that obtains cells from all epithelial layers[26]. The method involves opening the brush to expose bristles and carefully swiping it along the tissue layer. The brush with desired cells is cut from the catheter and placed in fixative, allowing it to agitate to dislodge tissues[26].
Slide Preparation
[edit]Immediately after sample extraction, the brush, containing the samples, is smeared directly onto a glass slide. It is followed by wet fixation using absolute alcohol[27], which stabilises the cells, prevents loss of cell contents and aids permeation of stains[28]. Staining creates drastic contrasts in cellular images, allowing pathologists to examine delicate structures closely. Both hematoxylin and eosin stain and Papanicolaou stain are well-adopted staining methods in cytological examination[27][29].
Bile duct cytogenetic examination analyses genetic material from bile duct cells, aiding diagnosis of biliary disorders and malignancies. Common approaches include fluorescence in situ hybridisation (FISH), next-generation sequencing (NGS), and investigation of microRNA.
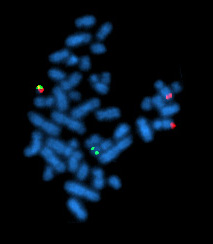
Fluorescence in situ hybridisation (FISH)
[edit]FISH is a molecular technique used to detect specific genetic abnormalities at a chromosomal level. It uses fluorescently labeled probes designed to bind to particular DNA sequences within the chromosomes of cells. When these probes attach to their target regions, they emit fluorescence, detected and visualised under a fluorescence microscope. FISH is particularly valuable for identifying aneuploidies, which are deviations from the normal number of chromosomes (46), as well as large inversions, deletions or duplications of chromosomal segments[1]. It commonly observes two types of chromosomal abnormalities, polysomy or monosomy[2].
Next-generation sequencing (NGS)
[edit]NGS is the process of using a DNA sequencer to read nucleotide base sequences. The latest models of DNA sequencers have high throughput, allowing the screening of thousands of genes simultaneously with great precision. A geneticist then interprets the sequences obtained to identify any pathogenic gene variants that predispose the subject to cancer. Common target genes of NGS in oncopathological studies are KRAS and TP53, which are tumour-suppressing genes. Often, a combination of mutations is found in malignant tumours[5][30].
MicroRNA
[edit]MicroRNAs (miR) are small, non-coding molecules that regulate mRNA expression, abundantly found in extracellular vesicles[11]. To obtain miRs, mRNA is first isolated from brush cytology samples and transcribed into miR using reverse transcription kits. Next, to reveal the amount of miR present in the sample, quantitative miR expression analysis is performed[31]. Certain miRs are specific to certain malignant, making them a distinctive biomarker in bile duct cancer with high diagnostic potential.
Other Methods
[edit]Immunocolorimetric ELISA
[edit]ELISA is a biochemistry assay that detects and quantifies the amount of target protein by making use of specific identification structures called antigens. Colour change occurs once antigens are detected in the reaction mixture. The colour intensity of the solution is measured using a colorimeter and can thus be used to infer the concentration of antigens[32]. Minichromosome maintenance proteins (MCM) are notable targets in cancer research. Given their involvement in DNA synthesis initiation, any dysregulation is highly indicative of premalignant or malignant tumours[5].
Result analysis in Bile Duct Cytology
[edit]Cellular Characteristics
[edit]
Benign cells
[edit]Benign cells are non-cancerous, slow-growing, and non-invasive[33]. They typically exhibit a picket-fence arrangement, with basally located nuclei and columnar, non-mucinous cytoplasm[34]. Such conditions are often linked to infiltrating inflammation, bile duct stones, and necrosis[3]. Looking at benign tissues as a whole, they tend to have smooth borders with tapered margins[7].

Dysplasia
[edit]Dysplasia conditions precede the formation of cancer, which is often referred to as premalignant lesions[34]. Common features include nuclear pseudostratification, distorted cell polarity, cribriforming, and abnormally large nuclei[35]. It is recommended to conduct bile duct brushing of the remaining bile duct to assess for any sub-clinical carcinomatous changes[36].

Malignant cells
[edit]Malignant cells are cancerous cells that divide uncontrollably and invade other tissues[4]. They present with features such as enlarged nuclei, anisonucleosis, meaning abnormal size of nucleus, loss of cellular polarity, and crowding or overlapping of cells[34]. Looking at malignant tissues as a whole, they are mostly irregular with shouldered margins[7]. To confirm the extent of malignancy and determine the stage of cancer, immediate imaging studies such as magnetic resonance imaging and endoscopic retrograde cholangiopancreatography should be conducted[37].
Background Assessment
[edit]Besides carcinoma, bile duct cytology also reveals background complications such as inflammation or necrosis of bile duct epithelial cells[3]. Inflammation of the bile duct is caused by reactive cells, such as cysts and infections[38]. Although the histological findings of bile duct cells are not specific, reactive bile duct cells are observed in sheets that maintain a monolayer appearance, exhibiting slight nuclear overlap, enlarged nuclei, smooth nuclear outlines, finely granular chromatin, and small, visible nucleoli[39].
Bile duct necrosis is a serious complication of localised death of bile duct epithelial cells[40]. Under microscopic view, a necrotic bile duct appears as a dark brown tubular structure with a large dark green cystic mass-like lesion[41]. It causes significant coagulation on the lumen, which exacerbates necrosis of peri-bile duct tissue[41]. The expansive spread of necrotic tissue may cause thrombosis of the portal vein, which runs along the bile duct[41]. Under endoscopic examination, thrombosis can be identified as a filling of the lumen by an unusual mass[42].
Diagnostic Challenges and Improvements
[edit]Sampling Error
[edit]Sampling errors remain the major reason for insensitivity or false positive results in brush biopsy[12]. Malignant cells cannot be identified because of technical challenges, including difficult anatomic sites, extensive fibrosis, poor visualisation, and the presence of benign epithelium covering the tumor[13]. A combination of brush cytology and forceps biopsy or endoscopic needle aspiration may be employed to improve diagnostic yield[13][43]. Utilising long cytobrushes to sample larger and longer areas of the biliary tract can increase cellularity to reduce false positives[43]. The cell-collecting technique should be optimised by determining whether to push or pull the brush through the sheath[13].
Misidentification of Malignancy
[edit]Misidentifying malignancy is a significant diagnostic challenge, particularly with well-differentiated carcinomas such as mucinous and papillary tumors[13]. These tumors can morphologically present as benign, leading to potential false-negative diagnoses[44]. Additionally, smear backgrounds with necrotic debris can obscure viable malignant cells, presenting another diagnostic pitfall[13]. Abundant inflammatory exudate can complicate the differentiation between necrosis related to tumors and inflammatory changes[13]. Cells that appear to be undergoing degenerative changes due to inflammation may also be mistakenly overlooked in malignant conditions[45]. With this ambiguity in mind, cytologists should pay attention to identifying susceptible cytological features to detect malignancy accurately.
History of Bile Duct Visualisation and Cytology
[edit]Development in visualising the bile duct
[edit]Intravenous Cholangiography
[edit]Introduced in 1953, intravenous cholangiography involves injecting hexa-iodo organic compounds into the bloodstream and visualising the biliary structure with laminography[46][14]. However, it is contraindicated in subjects with impaired hepatic functions, as such contrasting agents must undergo hepatic metabolism before being excreted by the body[14].
Percutaneous Transhepatic Cholangiography (PTC)
[edit]To tackle the above constraint, percutaneous transhepatic cholangiography (PTC) was proposed in 1956 as an alternative to intravenous cholangiography[15]. The subject is first put under anesthesia, and an organic iodine compound is injected into the biliary duct. X-ray visualises the bile duct and the image is examined for any abnormal occlusions[47][48]. This procedure risks puncturing the extrahepatic biliary system and passage of bile into blood, which may result in bile peritonitis and septic shock. One case of death has been recorded post-operation[47].
Development in collecting bile duct samples
[edit]Secretin Test
[edit]Secretin test has been utilised to test cholangiopancreatic function since the early 20th century[16]. Secretin is injected intravenously to stimulate pancreatic secretions and diagnose the condition within the biliary duct[49]. Cells are isolated from the secretion for staining, while the biliary pigment concentration is examined. Low pigment concentration indicates potential bile duct occlusion[50]. As newer methodologies emerge, this method is rendered obsolete in modern routines.
Endoscopic Retrograde Cholangiopancreatography with Bile Duct Cytology
[edit]The diagnostic potential of endoscopic retrograde cholangiopancreatography (ERCP) became apparent in 1975, when Osnes first performed ERCP with brush cytology[17][51]. Cells of the bile duct were collected directly for cytological examinations. The minimally invasive nature gains traction over time in detecting dysplastic cells before evolving into malignant carcinoma[17].
References
[edit]- ^ a b Gores, Gregory J. (2014-10-01). "Addressing unmet clinical needs: FISHing for bile duct cancer". Cancer Cytopathology. 122 (11): 789–790. doi:10.1002/cncy.21484. ISSN 1934-662X.
- ^ a b Halling, Kevin C.; Kipp, Benjamin R. (2007-07-16). "Fluorescence in situ hybridization in diagnostic cytology". Human Pathology. 38 (8): 1137–1144. doi:10.1016/j.humpath.2007.04.015.
- ^ a b c Avadhani, Vaidehi; Hacihasanoglu, Ezgi; Memis, Bahar; Pehlivanoglu, Burcin; Hanley, Krisztina Z; Krishnamurti, Uma; Krasinskas, Alyssa M; Osunkoya, Adeboye O; Daniels, Lauren M; Freedman, Alexa A; Goodman, Michael; Adsay, Volkan; Reid, Michelle D (2017-04-19). "Cytologic predictors of malignancy in bile duct brushings: a multi-reviewer analysis of 60 cases". Modern Pathology. 30 (9): 1273–1286. doi:10.1038/modpathol.2017.51. ISSN 0893-3952.
- ^ a b "Malignancy: MedlinePlus Medical Encyclopedia". medlineplus.gov. Retrieved 2025-04-14.
- ^ a b c d e f Kurfurstova, Daniela; Slobodova, Zuzana; Zoundjiekpon, Vincent; Urban, Ondrej (2023-12-04). "The contribution of new methods in cytology for increasing sensitivity in the diagnosis of extrahepatic bile duct lesions". Biomedical Papers. 167 (4): 309–318. doi:10.5507/bp.2023.041.
- ^ a b c Reddy, Yogananda; Willert, Robert P (2009-12-01). "Endoscopic ultrasound: what is it and when should it be used?". Clinical Medicine. 9 (6): 539–543. doi:10.7861/clinmedicine.9-6-539. ISSN 1470-2118. PMC 4952290. PMID 20095294.
- ^ a b c d e Maccioni, F.; Martinelli, M.; Al Ansari, N.; Kagarmanova, A.; De Marco, V.; Zippi, M.; Marini, M. (2010-08-14). "Magnetic resonance cholangiography: past, present and future: a review". European Review for Medical and Pharmacological Sciences. 14 (8): 721–725. ISSN 1128-3602. PMID 20707292.
- ^ a b c Curcio, Gabriele; Traina, Mario; Mocciaro, Filippo; Liotta, Rosa; Gentile, Raffaella; Tarantino, Ilaria; Barresi, Luca; Granata, Antonino; Tuzzolino, Fabio; Gridelli, Bruno (2012-02-10). "Intraductal aspiration: a promising new tissue-sampling technique for the diagnosis of suspected malignant biliary strictures". Gastrointestinal Endoscopy. 75 (4): 798–804. doi:10.1016/j.gie.2011.12.005.
- ^ a b c Sugimoto, Shinya; Matsubayashi, Hiroyuki; Kimura, Hirokazu; Sasaki, Keiko; Nagata, Kaori; Ohno, Sachiyo; Uesaka, Katsuhiko; Mori, Keita; Imai, Kenichiro; Hotta, Kinichi; Takizawa, Kohei; Kakushima, Naomi; Tanaka, Masaki; Kawata, Noboru; Ono, Hiroyuki (2015-05-07). "Diagnosis of bile duct cancer by bile cytology: usefulness of post-brushing biliary lavage fluid". Endoscopy International Open. 3 (4): E323–328. doi:10.1055/s-0034-1391666. ISSN 2364-3722. PMC 4554506. PMID 26357678.
- ^ a b Hormati, Ahmad; Jafari, Saeede; Jabbari, Amir; Pezeshki Modares, Mahdi; Afifian, Mahboubeh; Abasi, Ahmad; Ahmadpour, Sajjad; Sharifi, Ali Reza (2020-09-19). "Comparison between Brush Cytology and Forceps Biopsy under Fluoroscopic Guidance for the Diagnosis of Proximal Cholangiocarcinoma". Middle East Journal of Digestive Diseases. 12 (4): 246–251. doi:10.34172/mejdd.2020.189. ISSN 2008-5230. PMC 7859605. PMID 33564381.
- ^ a b Ueta, Eijiro; Tsutsumi, Koichiro; Kato, Hironari; Matsushita, Hiroshi; Shiraha, Hidenori; Fujii, Masakuni; Matsumoto, Kazuyuki; Horiguchi, Shigeru; Okada, Hiroyuki (2021-06-10). "Extracellular vesicle-shuttled miRNAs as a diagnostic and prognostic biomarker and their potential roles in gallbladder cancer patients". Scientific Reports. 11 (1): 12298. doi:10.1038/s41598-021-91804-0. ISSN 2045-2322. PMC 8192895. PMID 34112884.
- ^ a b Ding, Song-Ming; Lu, Ai-Li; Xu, Bing-Qian; Shi, Shao-Hua; Edoo, Muhammad Ibrahim Alhadi; Zheng, Shu-Sen; Li, Qi-Yong (2021-02-01). "Accuracy of brush cytology in biliopancreatic strictures: a single-center cohort study". Journal of International Medical Research. 49 (2): 0300060520987771. doi:10.1177/0300060520987771. ISSN 0300-0605. PMC 7876769. PMID 33557655.
- ^ a b c d e f g Kocjan, Gabrijela; Smith, Ann Nisbet (1997). "Bile duct brushings cytology: Potential pitfalls in diagnosis". Diagnostic Cytopathology. 16 (4): 358–363. doi:10.1002/(SICI)1097-0339(199704)16:4<358::AID-DC11>3.0.CO;2-J.
- ^ a b c Raskin, Howard F.; Moseley Jr., Robert D.; Kirsner, Joseph B.; Palmer, Walter L. (1961). "Carcinoma of the pancreas, biliary tract and liver: Part II". CA: A Cancer Journal for Clinicians. 11 (5): 166–181. doi:10.3322/canjclin.11.5.166. ISSN 1542-4863.
- ^ a b Zimmon, David S.; Chang, James; Clemett, Arthur R. (1979-05-01). "Advances in the Management of Bile Duct Obstruction: Percutaneous Transhepatic Cholangiography and Endoscopic Retrograde Cholangiopancreatography". Medical Clinics of North America. 63 (3): 593–609. doi:10.1016/S0025-7125(16)31690-X. ISSN 0025-7125.
- ^ a b Raskin, Howard F.; Moseley Jr., Robert D.; Kirsner, Joseph B.; Palmer, Walter L. (1961). "Carcinoma of the pancreas, biliary tract and liver: Part II". CA: A Cancer Journal for Clinicians. 11 (5): 166–181. doi:10.3322/canjclin.11.5.166. ISSN 1542-4863.
- ^ a b c Osnes, M.; A., Serck-Hanssen; and Myren, J. (1975-11-01). "Endoscopic Retrograde Brush Cytology (ERBC) ol the Biliary and Pancreatic Ducts". Scandinavian Journal of Gastroenterology. 10 (8): 829–831. doi:10.1080/00365521.1975.12097055. ISSN 0036-5521. PMID 1202615.
- ^ Afzalpurkar, Shivaraj; Giri, Suprabhat; Kasturi, Sunil; Ingawale, Sushrut; Sundaram, Sridhar (2023-04-01). "Magnetic resonance cholangiopancreatography versus endoscopic ultrasound for diagnosis of choledocholithiasis: an updated systematic review and meta-analysis". Surgical Endoscopy. 37 (4): 2566–2573. doi:10.1007/s00464-022-09744-3. ISSN 1432-2218.
- ^ Curcio, Gabriele; Traina, Mario; Mocciaro, Filippo; Liotta, Rosa; Gentile, Raffaella; Tarantino, Ilaria; Barresi, Luca; Granata, Antonino; Tuzzolino, Fabio; Gridelli, Bruno (2012-01-31). "Intraductal aspiration: a promising new tissue-sampling technique for the diagnosis of suspected malignant biliary strictures". Gastrointestinal Endoscopy. 75 (4): 798–804. doi:10.1016/j.gie.2011.12.005.
- ^ Ciocirlan, M.; Ponchon, T. (2004-02-06). "Diagnostic Endoscopic Retrograde Cholangiopancreatography". Endoscopy (in German). 36 (2): 137–146. doi:10.1055/s-2004-814181. ISSN 0013-726X.
- ^ Isayama, Hiroyuki; Tomishima, Ko; Ishii, Shigeto; Takasaki, Yusuke; Ushio, Mako; Fujisawa, Toshio (2025-01-01). "Endoscopic Ultrasound-guided Biliary Interventions". Techniques and Innovations in Gastrointestinal Endoscopy. 27 (2). doi:10.1016/j.tige.2025.250916. ISSN 2590-0307.
- ^ Arrivé, Lionel; Hodoul, Marianne; Arbache, Antoune; Slavikova-Boucher, Lucie; Menu, Yves; El Mouhadi, Sanaâ (2015-12-01). "Magnetic resonance cholangiography: Current and future perspectives". Clinics and Research in Hepatology and Gastroenterology. 39 (6): 659–664. doi:10.1016/j.clinre.2015.07.005. ISSN 2210-7401.
- ^ Vilmann, Peter (1996-01-01). "Endoscopic ultrasonography-guided fine-needle aspiration biopsy of lymph nodes". Gastrointestinal Endoscopy. 43 (2): S24 – S29. doi:10.1016/S0016-5107(96)81510-0. ISSN 0016-5107.
- ^ Akbar, Usman A.; Vorla, Mounica; Chaudhary, Ahmed Jamal; Fatima, Maurish; Vikash, Fnu; Taj, Sobaan; Qazi, Shaheryar; Khan, Zubair (2023-10-09). "Preventive Saline Irrigation of the Bile Duct to Reduce the Rate of Residual Common Bile Duct Stones Without Intraductal Ultrasonography: A Systematic Review and Meta-Analysis". Cureus. 15 (10): e46720. doi:10.7759/cureus.46720. ISSN 2168-8184. PMC 10630706. PMID 38021516.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Jang, Sung Ill; Nahm, Ji Hae; Lee, See Young; Jeong, Seok; Lee, Tae Hoon; Kim, Dong Uk; Kwon, Chang-Il; Cho, Jae Hee; Sung, Min Je (2024-11-08). "The Catheter Flushing Method Shows a Similar Diagnostic Yield to the Conventional Method in Brushing Cytology for Biliary Strictures". Journal of Clinical Medicine. 13 (22): 6741. doi:10.3390/jcm13226741. ISSN 2077-0383. PMC 11594799. PMID 39597885.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Brugge, WilliamR.; DeWitt, John; Klapman, JasonB.; Ashfaq, Raheela; Shidham, Vinod; Chhieng, David; Kwon, Richard; Baloch, Zubair; Zarka, Matthew; Staerkel, Gregg (2014). "Techniques for cytologic sampling of pancreatic and bile duct lesions: The Papanicolaou Society of Cytopathology Guidelines". CytoJournal. 11 (2): 9. doi:10.4103/1742-6413.133311. ISSN 1742-6413.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ a b Volmar, Keith E.; Vollmer, Robin T.; Routbort, Mark J.; Creager, Andrew J. (2006). "Pancreatic and bile duct brushing cytology in 1000 cases". Cancer Cytopathology. 108 (4): 231–238. doi:10.1002/cncr.21842. ISSN 1097-0142.
- ^ Archibugi, Livia; Mariani, Alberto; Ciambriello, Biagio; Petrone, Maria Chiara; Rossi, Gemma; Testoni, Sabrina Gloria Giulia; Carlucci, Michele; Aldrighetti, Luca; Falconi, Massimo; Balzano, Gianpaolo; Doglioni, Claudio; Capurso, Gabriele; Arcidiacono, Paolo Giorgio (2020-10-21). "High sensitivity of ROSE-supported ERCP-guided brushing for biliary strictures". Endoscopy International Open. 09 (03): E363 – E370. doi:10.1055/a-1322-2638. ISSN 2364-3722. PMC 7895655. PMID 33655035.
- ^ Jörundsson, Einar; Lumsden, John H.; Jacobs, Robert M. (2009-02-23). "Rapid Staining Techniques in Cytopathology: A Review and Comparison of Modified Protocols for Hematoxylin and Eosin, Papanicolaou and Romanowsky Stains". Veterinary Clinical Pathology. 28 (3): 100–108. doi:10.1111/j.1939-165X.1999.tb01057.x. ISSN 0275-6382.
- ^ Harbhajanka, Aparna; Michael, Claire W.; Janaki, Nafiseh; Gokozan, Hamza N.; Wasman, Jay; Bomeisl, Philip; Yoest, Jennifer; Sadri, Navid (2020-05-15). "Tiny but mighty: use of next generation sequencing on discarded cytocentrifuged bile duct brushing specimens to increase sensitivity of cytological diagnosis". Modern Pathology. 33 (10): 2019–2025. doi:10.1038/s41379-020-0577-1.
- ^ Le, N.; Fillinger, J.; Szanyi, Sz.; Wichmann, B.; Nagy, Z. B.; Ivády, G.; Burai, M.; Tarpay, Á.; Pozsár, J.; Pap, Á.; Molnár, B.; Csuka, O.; Bak, M.; Tulassay, Z.; Szmola, R. (2019-09-01). "Analysis of microRNA expression in brush cytology specimens improves the diagnosis of pancreatobiliary cancer". Pancreatology. 19 (6): 873–879. doi:10.1016/j.pan.2019.04.001. ISSN 1424-3903.
- ^ Keane, Margaret G; Huggett, Matthew T; Chapman, Michael H; Johnson, Gavin J; Webster, George J; Thorburn, Douglas; Mackay, James; Pereira, Stephen P (2017-01-12). "Diagnosis of pancreaticobiliary malignancy by detection of minichromosome maintenance protein 5 in biliary brush cytology". British Journal of Cancer. 116 (3): 349–355. doi:10.1038/bjc.2016.447. ISSN 0007-0920. PMC 5294492. PMID 28081547.
- ^ Cleveland Clinic (2024-08-15). "Benign Tumor: Definition, Types, Causes & Management".
- ^ a b c Themes, U. F. O. (2019-03-31). "Diagnostic Cytology of the Biliary Tract and Pancreas". Abdominal Key. Retrieved 2025-04-02.
- ^ Liu, Yongjun; Yeh, Matthew M. (2022-06-14). "Bile duct dysplasia and associated invasive carcinoma: clinicopathological features, diagnosis, and practical challenges". Human Pathology. 132: 158–168. doi:10.1016/j.humpath.2022.06.012.
- ^ Adsay, N. Volkan; Basturk, Olca (2023-11-17). "Dysplasia and Early Carcinoma of the Gallbladder and Bile Ducts". Gastroenterology Clinics of North America. 53 (1): 85–108. doi:10.1016/j.gtc.2023.10.001.
- ^ Lee, Sang-Hoon; Song, Si Young (2024-05-01). "Recent Advancement in Diagnosis of Biliary Tract Cancer through Pathological and Molecular Classifications". Cancers. 16 (9): 1761. doi:10.3390/cancers16091761. ISSN 2072-6694.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ Virgile, Jennifer; Marathi, Rachana (2025), "Cholangitis", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 32644372, retrieved 2025-04-11
- ^ Centeno, Barbara A (2023-03-01). "Cytopathology of Inflammatory Lesions of the Pancreatobiliary Tree". Archives of Pathology & Laboratory Medicine. 147 (3): 267–282. doi:10.5858/arpa.2021-0595-RA. ISSN 1543-2165.
- ^ Di Muzio, Bruno; Fortson, Benjamin; Baba, Yahya (2018-07-12), "Biliary necrosis", Radiopaedia.org, Radiopaedia.org, doi:10.53347/rid-61648, retrieved 2025-04-14
- ^ a b c Kobayashi, Satoshi; Kozaka, Kazuto; Gabata, Toshifumi; Matsui, Osamu; Koda, Wataru; Okuda, Miho; Okumura, Kenichiro; Sugiura, Takumi; Ogi, Takahiro (2020-09-11). "Pathophysiology and Imaging Findings of Bile Duct Necrosis: A Rare but Serious Complication of Transarterial Therapy for Liver Tumors". Cancers. 12 (9): 2596. doi:10.3390/cancers12092596. ISSN 2072-6694.
{{cite journal}}: CS1 maint: unflagged free DOI (link) - ^ "Portal Vein Thrombosis Imaging: Practice Essentials, Radiography, Computed Tomography". Medscape. 2023-11-16.
- ^ a b Geramizadeh, Bita; Moughali, Maryam; Shahim-Aein, Atefeh; Memari, Soghra; Ghetmiri, Ziba; Taghavi, Alireza; Bagheri Lankarani, Kamran (2018). "False negative and false positive rates in common bile duct brushing cytology, a single center experience". Gastroenterology and Hepatology from Bed to Bench. 11 (4): 296–300. ISSN 2008-2258. PMC 6204244. PMID 30425807.
- ^ Jackman, Roger J.; Marzoni, Francis A.; Rosenberg, Jarrett (2012-11-23). "False-Negative Diagnoses at Stereotactic Vacuum-Assisted Needle Breast Biopsy: Long-Term Follow-Up of 1,280 Lesions and Review of the Literature". American Journal of Roentgenology. 192 (2): 341–351. doi:10.2214/AJR.08.1127. ISSN 0361-803X.
- ^ Pantanowitz, Liron; Thompson, Lester D. R.; Rossi, Esther Diana (2018-03-09). "Diagnostic Approach to Fine Needle Aspirations of Cystic Lesions of the Salivary Gland". Head and Neck Pathology. 12 (4): 548–561. doi:10.1007/s12105-018-0904-8. ISSN 1936-055X.
- ^ Frommhold, W. (1953-09-01). "[A new type contrast medium for intravenous cholecystography]". Fortschritte Auf Dem Gebiete Der Rontgenstrahlen. 79 (3): 283–291. PMID 13107811.
- ^ a b Raskin, Howard F.; Moseley Jr., Robert D.; Kirsner, Joseph B.; Palmer, Walter L. (1961). "Carcinoma of the pancreas, biliary tract and liver: Part II". CA: A Cancer Journal for Clinicians. 11 (5): 166–181. doi:10.3322/canjclin.11.5.166. ISSN 1542-4863.
- ^ KIDD, HENRY A. (1956-02-01). "Percutaneous Transhepatic Cholangiography". A.M.A. Archives of Surgery. 72 (2): 262–268. doi:10.1001/archsurg.1956.01270200078014. ISSN 0096-6908.
- ^ Dreiling, David A.; Nieburgs, Herbert E.; Janowitz, Henry D. (1960-05-01). "The Combined Secretin and Cytology Test in the Diagnosis of Pancreatic and Biliary Tract Cancer". Medical Clinics of North America. 44 (3): 801–815. doi:10.1016/S0025-7125(16)34013-5. ISSN 0025-7125.
- ^ Dreiling, David A.; Nieburgs, Herbert E.; Janowitz, Henry D. (1960-05-01). "The Combined Secretin and Cytology Test in the Diagnosis of Pancreatic and Biliary Tract Cancer". Medical Clinics of North America. 44 (3): 801–815. doi:10.1016/S0025-7125(16)34013-5. ISSN 0025-7125.
- ^ Lahori, Mega; Andotra, Urvashi; Malhotra, Aneeta Singh (2022-05-04). "Cytology of Bile Duct Brushings: Streaming Ahead with Time". Annals of Pathology and Laboratory Medicine. 9 (4): R1–8. doi:10.21276/apalm.3163. ISSN 2349-6983.


