User:IamsadXD/sandbox
Cannabis Arteritis
[edit]Cannabis arteritis is a rare disease that occurs when there is long-term cannabis consumption. The disease is characterized by swelling and blockages in blood vessels, especially in the arteries, which bring blood from the heart to all parts of the body. [1]
Cannabis arteritis is not only associated with using cannabis. Patients with cannabis arteritis often do not only consume cannabis but also tobacco.[2] Researchers hypothesize that a toxic substance common between the two - arsenic, might be the factor causing this condition.[1]
As the mechanism of the disease is not well-known, it is usually diagnosed by exclusion, meaning to arrive at this diagnosis after all other possible diseases are excluded.[3] After diagnosis, a common treatment is to stop using cannabis, along with medications that help restore blood flow (such as vasodilators, antiplatelet agents, etc.). If the case is serious, surgeries might be done to remove the affected body part completely (amputation). [1] [4]
Cannabis arteritis rarely occurs, first reported in 1960, it mostly affects young adults, especially men. There are only around 50 cases reported. [5] Researchers suspect there are still numerous cases not being diagnosed, along with the legalization of cannabis in different regions, and the rise in cannabis consumption, the disease has growing relevance. [6][7]
Associated Factors
[edit]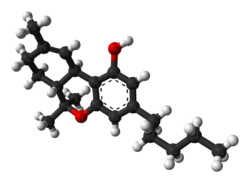
Unclear Mechanisms
[edit]The current understanding of cannabis arteritis is not sufficient to explain the underlying mechanism between cannabis smoking and cannabis arteritis.[2] However, the main psychoactive component of cannabis, Δ9-tetrahydrocannabinol (THC), is implicated in the disease's pathogenesis,[2] meaning that there is a correlation between cannabis smoking and the disease. Through experimenting with animal models, studies suggest that THC may exert a vasoconstrictive effect, potentially mediated through adrenergic pathways.[8]
Tobacco Use as a Confounding Factor
[edit]However, the use of tobacco has made the identification of the cause more complicated. Among the reported cases, most case reports (97%) showed associated tobacco smoking. [2] This raises a concern about the synergistic interaction between the two substances, and it might act as a confounding factor for the relationship between cannabis and cannabis arteritis.
Potential Contribution of Arsenic Contamination
[edit]Besides, these two substances share a common potential contaminant called arsenic, which has been hypothesized to contribute to vascular toxicity, meaning it could be the factor causing this condition.[1][9] On top of that, arsenic could inhibit vascular endothelial growth factor (VEGF) and induce endothelial cell apoptosis.[5] The inhibition of VEGF disrupts endothelial cells' ability to repair form new blood vessels, which makes the condition worsen, as the body already struggles with blood flow due to the disease. Meanwhile, the apoptosis of endothelial cells reduces the functional lining of blood vessels, thus reducing the ability to dilate and deliver blood.
Symptoms
[edit]Raynaud's Phenomenon
[edit]Symptoms of cannabis arteritis often involve fingers, toes, etc. The earliest sign of having cannabis arteritis is often reflected by Raynaud's phenomenon, which is characterized by the change in color (turning white, blue or red) in these extremities, white due to lack of blood flow, blue due to loss of oxygen when cold, and red when warmed up and circulation returns. [10][11]
Progression to Ulceration and Necrosis
[edit]As the condition worsens, patients may further develop symptoms such as ulcerations, which then evolve into necrosis, also affecting the toes and fingers, and inducing pain.[9] These symptoms result from chronic ischemia caused by the arterial inflammation caused by the disease and could lead to tissue death if the blood flow continues to be blocked by the inflammation. In serious cases, the prolonged lack of blood flow could lead to the severe complications mentioned (gangrene, digital necrosis, etc.), which then require amputations as the affected limb tissues have lost their function.
Loss of Distal Pulses and Venous Thrombosis
[edit]Apart from those symptoms, the early disappearance of distal pulses - pulses at the wrist and around the feet, could be observed in cannabis arteritis patients.[10] Venous thrombosis, a type of blood clot occurring in the veins (e.g. deep vein thrombosis, lower limb superficial vein thrombosis, etc.), was also observed in some patients. [10]
The severity and presentation of symptoms are influenced by factors like the duration of cannabis consumption, the usage of tobacco, and the vascular health of the patient.
Diagnosis
[edit]Clinical Evaluation and Patient History
[edit]Diagnosis of cannabis arteritis relies on a combination of clinical evaluation, patient history, and imaging studies. For instance, a key component is a documented history of chronic, heavy cannabis use, often verified through patient reporting or toxicological analysis of biological samples.[2] Moreover, clinicians may inquire about the duration and frequently of cannabis use to establish a pattern, as prolonged exposure is strongly associated with vascular changes. To be specific, individuals with a record of cannabis use extending over multiple years or daily consumption have a much higher risk. Note that symptoms likeas pain, numbness, coldness, or discoloration in the extremities are prevalent among patients[1] These may worsen with activity or cold exposure.
Diagnostic Confirmation
[edit]With the aim of confirmation, other potential causes of peripheral vascular disease, which includes atherosclerosis, autoimmune conditions, and Buerger’s disease must be excluded through medical assessment.[4] To be specific, blood tests for autoimmune markers and lipid profiles can help differentiate these conditions while imaging techniques, such as angiography or Doppler ultrasound, are employed to identify characteristic vascular abnormalities. This includes segmental occlusions or stenoses in small- to medium-sized arteries.[5] Concurrently, computed tomography (CT) angiography may occasionally be used to provide detailed visualization of arterial narrowing. Nevertheless, as there are no specific diagnostic test for cannabis arteritis, it is often identified through a process of exclusion[2] and adopting a meticulous approach can avoid misdiagnosis, as symptoms may mimic those of other vasculopathies.
Treatment
[edit]Medical and Supportive Therapies
[edit]The primary treatment for cannabis arteritis is the complete cessation of cannabis use, which is essential to prevent further progression.[2] For instance, patients are referred to counseling and support programs to address dependency, which ensures sustained abstinence. Beyond this foundational step, additional therapies are utilized based on the severity of the condition, e.g. vasodilators like prostacyclin can be administered to enhance blood flow to the affected areas.[1] Similarly, calcium channel blockers are used in some conditions to relieve vasospasm and antiplatelet agents, such as aspirin, which is often prescribed to reduce the risk of thrombosis.[4] Note that in cases involving ischemic tissue damage, hyperbaric oxygen therapy may be applied to promote healing.[5]
Surgical Interventions
[edit]Yet, in advanced cases where significant tissue loss has occurred, surgical interventions, e.g. amputation may become necessary.[2] Hence, procedures like bypass grafting may be attempted to restore circulation before resorting to amputation, but the effectiveness of these treatments varies, and complete reversal of the condition may not be possible. This happens in particularly when diagnosis and intervention are delayed.[1] Additionally, post-treatment monitoring is crucial to detect complications early, e.g. infection or further vascular compromise.
Prognosis
[edit]Factors Influencing Outcome
[edit]The prognosis for patients depends on several factors, which includes the timing of diagnosis, the extent of vascular damage, and the patient’s adherence to abstaining from cannabis use. For cases with early detection, followed by cessation of cannabis consumption, symptoms may improve, and further disease progression can be arrested.[2]
Risks of Advanced Cases
[edit]Still, in advanced cases, significant interventions like amputation may be required. This can potentially lead to long-term impacts on limb function.[5] Studies suggest that up to 30% of patients with severe presentations may require amputation despite treatment[4] and there is a notable risk of recurrence if cannabis use resumes.[1] Therefore, sustained abstinence from cannabis is critical to managing the condition while preventing further complications.[2]
Epidemiology
[edit]Prevalence and Risk Factors
[edit]Cannabis arteritis is considered a rare condition, with fewer than fifty cases documented in medical literature in recent years.[2] Specifically, it predominantly affects young adults, with a higher prevalence among men[1] and the primary risk factor is chronic, heavy cannabis use.[4] Although some affected individuals also use tobacco, cases have been reported in non-tobacco users, indicating that cannabis can independently trigger the condition.[5]
Potential for Increased Cases
[edit]Meanwhile, with the rising prevalence of cannabis use, particularly in regions where it has been legalized for medical or recreational purposes, there is potential for an increase in reported cases.[2] Nevertheless, the lack of large-scale epidemiological studies means that precise incidence rates remain unavailable.[4] The condition may be under-diagnosed or misdiagnosed due to its similarity to other peripheral vascular diseases and because healthcare providers may not routinely associate cannabis use with vascular pathology.[1]
History
[edit]Historical Background
[edit]Cannabis arteritis was first reported in 1960 by Sterne and Ducastaing, in an article named "Arteritis caused by Cannabis indica" published in Arch Mal Coeur Vaiss (PubMed). [12] The disease is thought to be resembling the Buerger's disease, a tobacco-related disorder, and is still classified as a particular form of Buerger's disease for some places as of the mid-2020s. [1]
Growing Awareness
[edit]Then in the 2000s, along with the accumulating number of cannabis arteritis cases (accumulating to around 50 cases [5]), the number of research articles and case reports also increased.
Present-day Relevance
[edit]As of the mid-2020s, cannabis arteritis remains a rare condition. However, researchers suspect that there are still many cases of cannabis arteritis not being diagnosed.[6] With the increasing trend of cannabis consumption, this disease becomes more and more relevant.
References
[edit]- ^ a b c d e f g h i j k Combemale, P.; Consort, T.; Denis-Thelis, L.; Estival, J-L.; Dupin, M.; Kanitakis, J. (January 2005). "Cannabis arteritis". British Journal of Dermatology. 152 (1): 166–169. doi:10.1111/j.1365-2133.2005.06340.x.
- ^ a b c d e f g h i j k l Cottencin, Olivier; Karila, Laurent; Lambert, Marc; Arveiller, Catherine; Benyamina, Amine; Boissonas, Alain; Goudemand, Michel; Reynaud, Michel (December 2010). "Cannabis Arteritis: Review of the Literature". Journal of Addiction Medicine. 4 (4): 191–196. doi:10.1097/ADM.0b013e3181beb022. ISSN 1932-0620.
- ^ Banana, Youssef; Bashir, Husam; Boukabous, Sara; Rezziki, Abdellah; Benzirar, Adnane; El Mahi, Omar (April 2022). "Cannabis arteritis: A case report and brief review of the literature". Annals of Medicine and Surgery (2012). 76: 103523. doi:10.1016/j.amsu.2022.103523. ISSN 2049-0801. PMC 9052130. PMID 35495400.
- ^ a b c d e f Noël, Bernard; Ruf, Isabelle; Panizzon, Renato G. (2008-05-01). "Cannabis arteritis". Journal of the American Academy of Dermatology. 58 (5, Supplement 1): S65 – S67. doi:10.1016/j.jaad.2007.04.024. ISSN 0190-9622.
- ^ a b c d e f g El Omri, Naoual; Eljaoudi, Rachid; Mekouar, Fadwa; Jira, Mohammed; Sekkach, Youssef; Amezyane, Taoufik; Ghafir, Driss (2017). "Cannabis arteritis". The Pan African Medical Journal. 26: 53. doi:10.11604/pamj.2017.26.53.11694. ISSN 1937-8688. PMC 5398854. PMID 28451030.
- ^ a b Santos, Rui Pedro; Resende, Cristina Isabel Pinho; Vieira, Ana Paula; Brito, Celeste (2017-03-13). "Cannabis arteritis: ever more important to consider". BMJ case reports. 2017: bcr2016219111. doi:10.1136/bcr-2016-219111. ISSN 1757-790X. PMC 5353368. PMID 28288999.
- ^ "World Drug Report 2022". United Nations : Office on Drugs and Crime. Retrieved 2025-04-01.
- ^ Grotenhermen, Franjo (2007). "The Toxicology of Cannabis and Cannabis Prohibition". Chemistry & Biodiversity. 4 (8): 1744–1769. doi:10.1002/cbdv.200790151. ISSN 1612-1880.
- ^ a b Pilitsi, Eleni; Kennamer, Brooke; Trepanowski, Nicole; Gonzalez, Reina; Trojanowski, Marcin; Phillips, Tania; Lam, Christina S. (2023-07-01). "Cannabis arteritis presenting with Raynaud's and digital ulcerations: a case-based review of a controversial thromboangiitis obliterans-like condition". Clinical Rheumatology. 42 (7): 1981–1985. doi:10.1007/s10067-023-06603-x. ISSN 1434-9949.
- ^ a b c Disdier, Patrick; Granel, Brigitte; Serratrice, Jacques; Constans, Joël; Michon-Pasturel, Ulrique; Hachulla, Eric; Conri, Claude; Devulder, Bernard; Swiader, Laure; Piquet, Philippe; Branchereau, Alain; Jouglard, Jacqueline; Moulin, Guy; Weiller, Pierre-Jean (January 2001). "Cannabis Arteritis Revisited: Ten New Case Reports". Angiology. 52 (1): 1–5. doi:10.1177/000331970105200101. ISSN 0003-3197.
- ^ Branch, NIAMS Science Communications and Outreach (2017-04-10). "Raynaud's Phenomenon". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Retrieved 2025-04-02.
- ^ Sterne, J.; Ducastaing, C. (February 1960). "[Arteritis caused by Cannabis indica]". Archives Des Maladies Du Coeur Et Des Vaisseaux. 53: 143–147. ISSN 0003-9683. PMID 13834494.

